| By Gale Staff |
As far as mental health conditions are concerned, borderline personality disorder (BPD) remains one of the most misunderstood. Each May, Borderline Personality Disorder Awareness Month challenges these misconceptions, bringing much-needed awareness to a condition that affects an estimated 1.4% of American adults.
For many, the road to diagnosis is long and confusing, with symptoms often mistaken for depression or anxiety or simply dismissed as “moodiness.”
Because BPD isn’t well-understood in the field of psychopathology, it complicates academic research. Gale Health and Wellness equips both professionals and students with centralized, up-to-date resources to support both advanced scholarship and entry-level exploration. The platform offers premier full-text reference works such as The Gale Encyclopedia of Medicine, and more than 630 topical articles from scholarly journals.
Misunderstandings within the medical field have also distorted the popular perception of BPD. Because the platform is also designed for non-experts, Gale Health and Wellness benefits the general public with its presentation of complex clinical terms in clear, stigma-free language and engaging multimedia content.
What Is Borderline Personality Disorder?
Borderline personality disorder is a complex mental health condition that disrupts emotional regulation, sense of self, and relational stability. At its root is a fear of abandonment that can make any perceived disconnection feel threatening.
People with BPD may react strongly when something in a relationship feels off, even if nothing is actually wrong. A delayed reply or a shift in someone’s tone might be enough to trigger the release of adrenaline and cortisol, which causes the body to enter a panic state. What follows can look like an overreaction, but the nervous system responds as if the threat were real.
In close relationships, these patterns can become especially intense. A person might form a strong attachment quickly, only to pull away as soon as that connection feels uncertain—even if that judgment is based on incomplete or erroneous information.
Many people with BPD experience a sense of identity that shifts depending on who they’re with, what’s happening around them, or how emotionally secure they feel at a given moment. While this behavior can sometimes be interpreted as inauthenticity, these identity shifts are an adaptive response that can develop when someone’s nervous system remains on high alert due to past trauma.
“Borderline personality disorder.” In The Gale Encyclopedia of Psychology, 4th ed., edited by Jacqueline L. Longe. Vol. 1. Farmington Hills, MI: Gale, 2022. Gale Health and Wellness (accessed May 7, 2025). https://link.gale.com/apps/doc/PC8273787053/HWRC?u=seoblogs&sid=bookmark-HWRC&xid=c28a2d16.
Childhood Attachment and Brain Development in BPD
Modern psychopathology attributes these patterns to two primary causes: neurological differences and attachment disruptions, both of which vary widely from person to person.
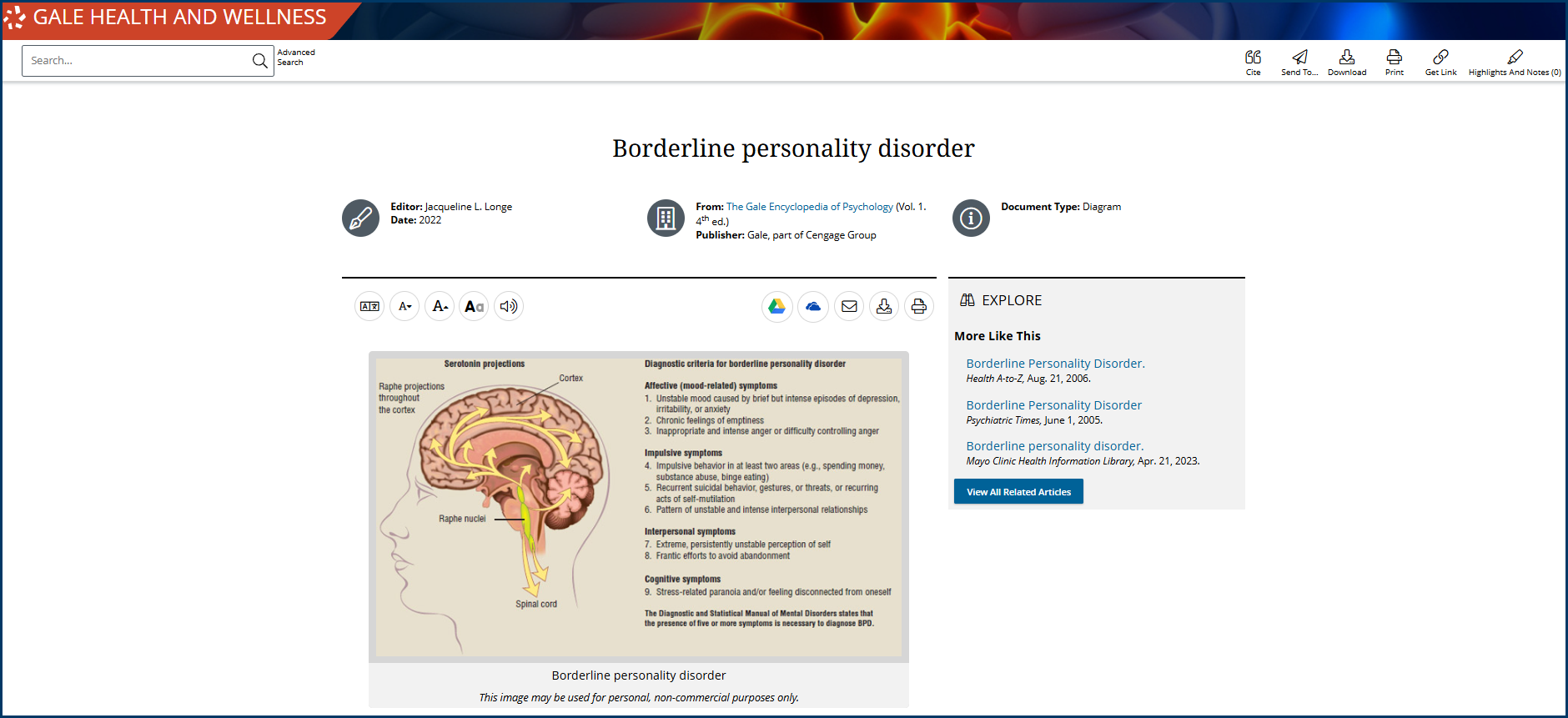
There’s growing evidence that BPD involves differences in how the brain processes emotion and threat. Neuropathic imaging has shown increased activity in the amygdala, the region involved in detecting danger and assigning emotional weight to experiences. At the same time, the prefrontal cortex—which helps regulate impulses and evaluate situations rationally—may be less active during moments of distress. This combination can make it harder for a person with BPD to downshift from emotional intensity once it starts.
Childhood trauma and unstable caregiver relationships also correlate to BPD later in life. According to attachment theory, a child’s early bond with caregivers teaches them how to regulate emotion and form secure connections. If that bond is inconsistent due to neglect or abuse, it can lead to an insecure attachment style and intense fight, flight, freeze, or fawn behaviors.
Common Misdiagnoses
The National Institutes of Health reports that approximately 40% of people with BPD are misdiagnosed at first, often sending them through a revolving door of ineffective medications and therapies.
One of the most common sources of confusion is bipolar disorder. Both conditions involve changes in mood and behavior, however key differences exist. Bipolar episodes usually last for days or weeks. They come in cycles, often without any apparent trigger, fluctuating between manic and depressive in a relatively predictable pattern. With BPD, someone can experience euphoria, disappointment, wrath, and peacefulness over a single day, often triggered by reactions to interpersonal relationships or other external stimuli.
For Academic Libraries: The Latest Research on Borderline Personality Disorder
BPD remains one of the most challenging conditions to research and teach. The condition doesn’t present the same way in every patient, and many of its core symptoms overlap with other diagnoses.
As a result, much of the most promising research no longer focuses on identifying standalone symptoms, but on understanding how they overlap and reinforce one another. Similarly, current research is moving toward assessing BPD through multiple fields—psychology, neuroscience, trauma studies, and even sociology—to build a complete picture of how the disorder functions and possible treatment options.
Gale Health and Wellness supports this work by providing access to full-text academic journal articles, current medical news, and interdisciplinary research. Unlike subscription-only journals, Gale offers a centralized, flexible research environment to support entry-level and advanced scholarship.
Comorbidity and Clinical Overlap
A 2024 study found that 83% of those diagnosed with BPD have co-occurring mood disorders, 85% have anxiety disorders, and 53% have other personality disorders. These comorbidities interact with one another, often amplifying the intensity of emotional dysregulation while also increasing the risk of misdiagnosis.
Does BPD Treatment Start with a Good Night’s Sleep?
Researchers are taking an increased interest in the relationship between insomnia and BPD’s core physiology. People with BPD often exhibit elevated nighttime cortisol levels, suggesting that their bodies remain in a heightened state of stress even during rest. This imbalance makes it much more difficult to enter REM sleep, the stage where our brains do the most work in emotional recovery and memory processing.
Todd, Carolyn. “While You’re at Rest, REM Sleep Gets to Work.” New York Times, March 7, 2023, D7(L). Gale Health and Wellness (accessed May 7, 2025). https://link.gale.com/apps/doc/A739803683/HWRC?u=seoblogs&sid=bookmark-HWRC&xid=1513e46a.
Sleep loss can impair emotional regulation. In individuals with BPD, whose baseline stress may already be elevated, chronic insomnia can intensify reactivity, delay emotional recovery, and diminish tolerance for everyday triggers.
Challenging Stigma with a Holistic Research Approach
BPD remains one of the most stigmatized psychiatric diagnoses, in part because its symptoms are often interpreted through a moral lens. Behaviors like emotional outbursts, boundary-pushing, or withdrawal are still labeled as “manipulative” or “non-compliant”—descriptions that assume intent rather than accounting for capacity.
Research, however, undermines these assumptions. When studied alongside data on sleep deprivation and chronic stress, behaviors that appear defiant or attention-seeking could be physiological symptoms of distress.
For those in clinical training, this holistic perspective challenges a purely psychological interpretation of BPD. A patient who seems emotionally volatile or unable to engage in therapy may be responding to biological strain. Sleep disruption doesn’t excuse emotional volatility but reframes how clinicians interpret it and the order in which they provide treatments. For example, a patient who isn’t sleeping likely won’t benefit from talk therapy until they’re getting enough rest to regulate emotions. Thus, patients may see better outcomes if treatments focus on an integrated model that prioritizes biological stability.
Students in fields like sociology and behavioral health who can access this research through Gale Health and Wellness are better equipped to understand the biological realities behind emotional dysregulation. That insight allows them to enter their fields prepared to advocate for systems of care that recognize those physiological burdens and respond to them more effectively.
Support for BPD Patients and Their Loved Ones
For people living with BPD—or supporting someone who is—credible, reader-friendly information can be hard to come by. Clinical summaries may be technically accurate but emotionally distant.
Gale Health and Wellness meets users where they are, offering medically-reviewed news articles, magazine features, and videos that also present emotional intelligence and real-world relevance. One example of the many user-friendly resources available for non-specialists is Lisa A. Phillips’s article “Tangled in Turmoil.”
The piece follows a woman navigating the emotional fallout of a disappearing partner as she uses Spanish-language videos to help explain her diagnosis. That moment—of being understood across both emotive and linguistic barriers—is something Gale Health and Wellness helps make possible with article translations available in more than 50 languages.
Finding Healthy Boundaries
Gale Health and Wellness’s video library includes firsthand stories that speak to the complicated realities of having relationships with loved ones living with BPD.
One of those stories appears in the video “To Save My Sister and Myself, I Had to Walk Away.” Sisters Kaitlin and Natalie reflect on what it took to rebuild their relationship after years of emotional exhaustion on both sides. Kaitlin, who was later diagnosed with BPD, describes living with emotions that “come in at 100 decibels”—a kind of sensory overload that made ordinary life feel urgent and chaotic.
While trying to help, Natalie stayed close for as long as she could. She listened, offered reassurance, and tried to carry Kaitlin’s pain alongside her. Eventually, it became too much. “I was losing myself,” Natalie says. “And I was starting to resent her.”
While taking some space helped, so did clarity about what was happening. The diagnosis gave Kaitlin a way to understand her reactions and take responsibility for managing them. It also gave Natalie the language to set limits without cutting her sister off.
The story of Kaitlin and Natalie, along with the many other resources available through Gale Health and Wellness, exemplify the importance of fostering both academic and empathetic understanding of BPD and other mental disorders.
To learn more about Gale Health and Wellness and how it can support mental health research in both academic and public libraries, please reach out to your local Gale sales representative.