| By Barbara Wexler, MPH |
Food allergies are more than just a dietary inconvenience—they’re a serious and growing public health issue that affects millions of people around the world. In the United States alone, an estimated 1 in 13 children has a food allergy, and adults aren’t immune either; some develop new food allergies well into adulthood. These reactions can range from mild irritation to full-blown medical emergencies. Whether you’re managing your own allergy or supporting someone else who is, understanding the basics can make all the difference.
At their core, food allergies are the result of a mistaken identity. A person’s immune system misinterprets a harmless food protein as a dangerous invader and mounts an attack. This immune response can happen when the person eats, touches, or even inhales particles from the offending food. It’s an immune system malfunction—and for those affected, it’s something they have to navigate every single day.
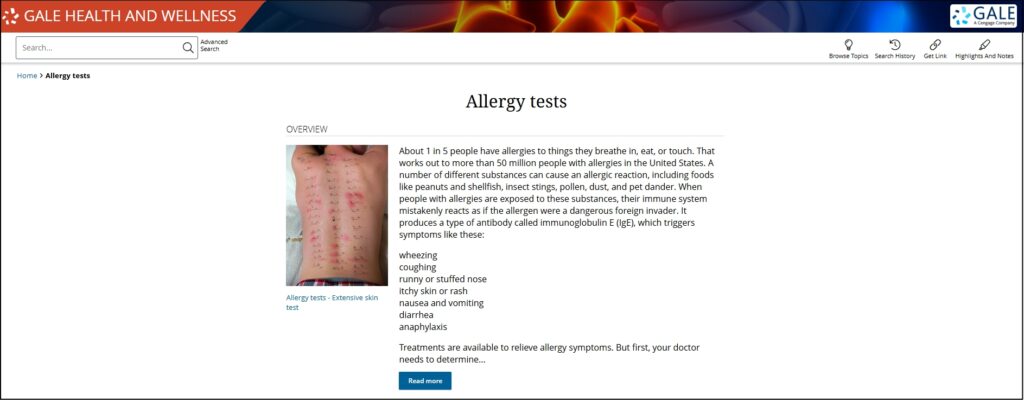
When someone with a food allergy is exposed to a trigger food, their immune system produces antibodies called immunoglobulin E (IgE). These antibodies stimulate the release of chemicals like histamine, which cause the typical allergy symptoms: swelling, hives, digestive issues, and even trouble breathing. Why does this happen in some people and not others? Scientists believe it’s a combination of genetics and environmental factors. If a child has one or more parents with allergies, their own chances of developing allergies go up significantly.
But not every bad reaction to food is a food allergy, even though people often use the terms interchangeably. It’s important to understand the difference. A food sensitivity or intolerance doesn’t involve the immune system. Instead, it usually stems from difficulty digesting a certain food. For example, someone with lactose intolerance lacks the enzyme needed to break down lactose, a sugar found in milk. This can cause bloating, cramping, and other unpleasant symptoms, but it’s not dangerous in the way a true allergy can be.
On the other hand, a food allergy can be life-threatening. That’s why it’s so important to get a proper diagnosis—what seems like a mild upset stomach could signal something far more serious if an allergy is involved.
Symptoms of a food allergy can appear within minutes or up to two hours after eating the problematic food. They can range from mild to severe, and they often escalate quickly. Common symptoms include:
- Itching or tingling in the mouth
- Swelling of the lips, tongue, throat, or face
- Hives or red, itchy skin
- Shortness of breath or wheezing
- Nausea, vomiting, or diarrhea
- Dizziness or fainting
The most serious kind of allergic reaction is called anaphylaxis. This is a medical emergency that can cause the throat to swell shut, blood pressure to plummet, and breathing to stop. Without immediate treatment, it can be fatal. That’s why people with known allergies often carry an epinephrine auto-injector like an EpiPen—it can save lives in a crisis.
When someone is having a severe allergic reaction, every second counts. The auto-injector delivers a dose of epinephrine (adrenaline) that can rapidly reverse the symptoms of anaphylaxis.
If you or someone near you is experiencing a suspected food allergy reaction:
- Ask if they have an epinephrine auto-injector and assist them to use it.
- Call 911 immediately, even if symptoms seem to improve.
- Lay the person flat and raise their legs, unless they’re vomiting or having trouble breathing—in which case they should sit up or lie on their side.
- Do not give them anything to eat or drink.
- Stay with them until emergency help arrives.
In the U.S., the majority of food allergy reactions are caused by just nine foods. The most common culprits are:
- Milk
- Eggs
- Peanuts
- Tree nuts (such as almonds, cashews, and walnuts)
- Soy
- Wheat
- Fish
- Shellfish
- Sesame
The FDA requires these allergens to be clearly labeled on packaged food, which helps people make safer choices at the grocery store and in restaurants.
Unfortunately, there’s no cure for food allergies yet. The only proven strategy is strict avoidance of the triggering food. Some children outgrow certain allergies over time—especially to milk, egg, and soy—but other allergies, especially peanut and shellfish, tend to stick around for life.
Ongoing medical research is also exploring promising therapies like oral immunotherapy, which involves gradually introducing small amounts of an allergen under medical supervision to build tolerance.
Not too long ago, the prevailing wisdom was to delay introducing allergenic foods like peanuts and eggs until a child was older. The idea was to give their immune systems time to mature. However, landmark research—most notably the LEAP study (Learning Early About Peanut Allergy)—has dramatically shifted this thinking.
We now know that early introduction of potentially allergenic foods, usually at around four to six months of age, can help prevent allergies from developing in the first place. This is particularly true for children considered high-risk—those with eczema or a family history of allergies. Parents should always speak with a pediatrician before introducing these foods, especially if the child has any existing health concerns.
This shift in thinking has major implications. Rather than avoiding allergenic foods, we now have a window of opportunity to build tolerance early—something that could change the trajectory of a child’s health.
Food allergies aren’t something to take lightly. They can affect every meal, every snack, and every social situation that involves food. But with the right knowledge, tools, and preparation, people with food allergies can live full, healthy lives. The key is awareness: understanding the difference between an allergy and a sensitivity, learning to recognize the signs of a reaction, and knowing how to respond when time is of the essence.
More good news is that prevention strategies are evolving. What once seemed like an inevitability—living with food allergies for life—is now being challenged with new research-backed approaches. Whether you’re a parent trying to protect your child, a teacher supporting a student, or someone managing your own allergy, staying informed is your first line of defense.
For more information on this topic, please see the “Food allergies” portal in the Gale Health and Wellness database:
These related portals will also be of interest:
Allergies
Allergy tests