Across the United States, an estimated 15.5 million adults and 7 million children live with attention-deficit/hyperactivity disorder (ADHD). This condition causes differences in how the brain is wired to respond to time, tasks, and rewards.
Symptoms often resemble behavioral or motivational issues, such as daydreaming, forgetfulness, restlessness, impulsivity, and difficulty completing tasks. To the outside world, those behaviors can seem like defiance or lack of effort—but they’re driven by real neurological differences, not personal choice.
When people misread the signs of ADHD, they often respond with judgment or punishment for behaviors the individual can’t control—especially in children, but also in adults. The assumption becomes that the person needs more discipline or motivation rather than considering that something else may be going on neurologically. That mindset makes it harder to recognize and address the underlying causes.
Public libraries can help clarify common misconceptions by making clinically accurate, reader-friendly information more accessible.
As a public health tool, Gale Health and Wellness is designed to deliver trustworthy information that meets a wide range of language and learning needs. Patrons can explore reference articles, clinical overviews, images, and videos available on the ADHD topic page. They can also listen to audio versions, adjust the display for readability, or translate content into more than 50 languages—features that help reduce barriers for everyone.
To guide your patrons toward trustworthy resources, we’ve created an overview of material from Gale Health and Wellness that explores how ADHD presents, what common symptoms can look like across age groups, and what to expect from an evaluation. For caregivers, we’ve also included support materials to help them have informed and affirming conversations with children and teens.
What Is ADHD?
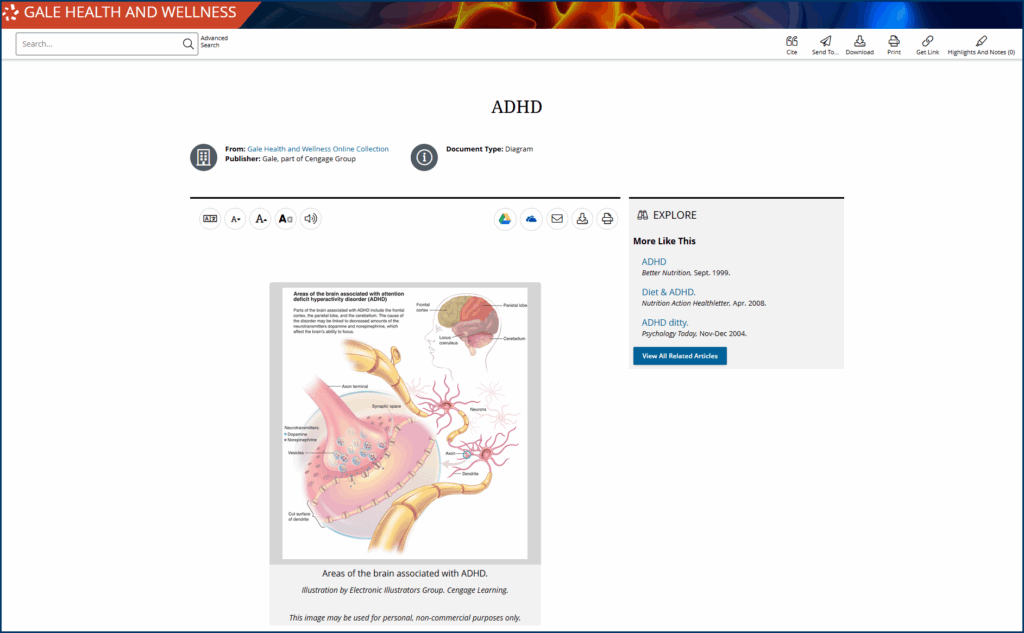
ADHD is a neurological condition that affects how the brain manages attention, motivation, and self-regulation.
For people with ADHD, specific brain networks develop and function differently—especially those that rely on dopamine. These networks help the brain assess how rewarding or urgent a task feels. When dopamine signaling is disrupted, as it is with ADHD, it can cause executive dysfunction, meaning that everyday tasks often fail to register as important or stimulating, even when the person understands their urgency.
As a result, a person may freeze when trying to start a task, regardless of its importance. They may struggle to stay focused if the payoff isn’t immediate, or feel stuck when asked to shift gears unexpectedly. These challenges reflect differences in how the brain processes and prioritizes information, rather than laziness or a lack of willpower.
While this is the neurological core of the condition, ADHD can look very different depending on the person and their stage of life.
ADHD Symptoms and Subtypes
The term ADD (attention-deficit disorder) is still commonly used, primarily when referring to individuals who appear distracted or disorganized but don’t outwardly present symptoms of hyperactivity-impulsivity. That terminology is outdated, however. Today, our understanding of the condition has brought all forms of the condition under the umbrella of ADHD.
In general, symptoms include:
- Feeling mentally stuck or unable to start tasks, even when they feel urgent (sometimes called task paralysis)
- Forgetting daily responsibilities, like returning calls or keeping appointments
- Struggling to stay focused on tasks that aren’t immediately interesting
- Avoiding responsibilities that require sustained mental effort
- Frequently losing track of what you were doing or saying
- Acting without thinking, especially in social situations
- Having trouble following multi-step instructions
- Difficulty managing time or meeting deadlines
- Feeling restless or unable to relax
Depending on the combination of symptoms, a professional can then categorize the presentation into one of three subtypes:
- Predominantly Inattentive Type: Struggle with focus, follow-through, memory, and organization. They may be described as spacey or forgetful rather than disruptive, which often leads to missed or delayed diagnoses.
- Predominantly Hyperactive-Impulsive Type: Characterized by excessive movement, restlessness, impulsivity, or difficulty sitting still. It tends to be more visible in classroom settings, which is one reason it’s more frequently diagnosed in young boys.
- Combined Type: The most common presentation includes symptoms of both inattention and hyperactivity-impulsivity.
For those interested in learning more about these symptoms and how they correlate to particular ADHD subtypes, life stages, or demographics, Gale Health and Wellness offers detailed clinical overviews and multimedia content that break down key differences in clear, accessible language.
The Myth of ADHD as a Modern Phenomenon
One of the most persistent misconceptions about ADHD is that it’s a product of modern lifestyles—caused by too much screen time, poor nutrition, or inconsistent parenting.
As further “proof,” some people point to the rise in diagnosis rates over the past two decades. Data from the CDC shows that approximately 11.3% of US children ages 5–17 have received an ADHD diagnosis, up from roughly 6% in the late 1990s. Among adults, about 6% currently have a diagnosis, representing a growth rate of 123.3% since 2007.
However, correlation does not imply causation. Despite the upward trend in diagnoses, population-wide studies suggest that the actual prevalence of ADHD has remained relatively stable.
What has changed is our ability to recognize ADHD more accurately, particularly in how symptoms manifest in different populations. At the same time, stigma around seeking help has decreased. As a result, more people—particularly adults, women, and people of color—are being identified and diagnosed today than in the past.
ADHD is a highly heritable, brain-based condition with well-documented neurological features. Blaming symptoms on sugar and screen time doesn’t just miss the point, it draws attention away from interventions that actually help. These misconceptions can make it harder for people to recognize the condition in themselves or others, delaying support that could make daily life more manageable.
Getting Evaluated for ADHD: What to Expect
An ADHD diagnosis isn’t based on a single test. It’s a comprehensive process that examines patterns of behavior over time and across various settings, allowing healthcare providers to gather information from multiple sources.
For children, this often includes:
- Academic evaluations or classroom observations, if available
- Rating scales to assess symptoms across environments
- Detailed input from caregivers and teachers
- A developmental and medical history
For adults, the diagnostic process may include:
- A self-reported history of symptoms, including retrospective questions about childhood
- Screening for other conditions that may affect attention, memory, or mood
- Input from close family or partners, when possible
In some cases, especially when symptoms are complex or overlap with those of other conditions, a psychologist, psychiatrist, or neurologist may be consulted to conduct a more in-depth evaluation. Some families also work with educational psychologists to clarify how ADHD may affect learning or academic performance.
Supporting Children Through an ADHD Diagnosis
It’s normal for kids to get distracted—to forget directions, test boundaries, and melt down over homework now and then. One of the most common questions caregivers ask is, “How do I know if this is ADHD or just typical kid behavior?”
The answer often comes down to persistence and impact. Most kids have difficult days now and then. For those with ADHD, the challenges tend to follow a consistent pattern. In such instances, difficulties with concentration and staying on task typically:
- Show up across multiple settings—not just at home, or at school
- Interfere with learning, relationships, or daily routines
- Continue over time, even with structure and support
Gale Health and Wellness can help families explore what ADHD is—and isn’t—before taking the next step with a medical provider. If these patterns feel familiar, it may be time to consider an evaluation.
Understanding the Diagnosis
When a child is diagnosed with ADHD, it’s natural for caregivers to feel relief and uncertainty at the same time. The diagnosis can validate what you’ve already sensed: your child isn’t lazy, defiant, or bad at listening—they’re wired differently. Now, you have a starting point to build support for the child with accommodations and evidence-based interventions.
Children and teens with ADHD are often painfully aware that something feels harder for them. Before a diagnosis, many internalize negative messages—about being lazy, bad at school, “too much,” or not trying hard enough. A diagnosis can bring relief, but it can also trigger fear and confusion. It’s vital that parents and guardians have conversations about what it means to have ADHD.
Talking to Younger Children About ADHD
For younger children, there’s no need to explain brain chemistry. What matters is helping them see that their brain works differently, not incorrectly. Use language that’s simple and affirming to help them name what they’re experiencing:
- “Your brain likes to think fast. That’s why it’s hard to slow down sometimes.”
- “It takes more energy for your brain to switch between tasks. That’s not your fault.”
- “You’re not doing anything wrong. Your brain just needs different tools to help it focus.”
Gale Health and Wellness also provides a list of children’s books that can make the conversation a little easier.
Supporting Tweens and Teens
A later diagnosis opens the door to more direct, honest conversations—but it can also bring up complicated emotions. Older adolescents may feel like they’ve been struggling without support, or that others misunderstood them for years. Some may worry that the diagnosis will change how others see them. Others might feel relieved to finally have an explanation.
All of those reactions are valid. Help them name what they’re feeling, then offer reassurance about what the diagnosis does (and doesn’t) mean.
You might say:
- “It’s OK to feel frustrated that this didn’t come sooner. What matters now is that we can move forward with better support.”
- “This diagnosis doesn’t define you. It helps explain why some things have been harder, and how we can work with your brain—not against it.”
- “You’re still you. Knowing that you have ADHD doesn’t take anything away from that, it just gives us more ways to help you feel successful and supported.”
- “Feeling confused or upset is completely normal. You’re allowed to take your time with this.”
It’s also important to counteract the belief that ADHD limits a child’s future. While the transition from school to work can be more challenging, people with ADHD can thrive as creative and resourceful adults, especially when supported in environments that understand their needs.
For kids and teens to attain a happy, prosperous future—whatever that might look like for them—they first need to believe that it’s a possibility. Support and understanding from the adults in their lives can go a long way to make this happen.
Reach out to your local Gale representative to learn more about how Gale Health and Wellness can support ADHD awareness, enhance community health literacy, and help your patrons lead more informed and empowered lives.